Prior to the Covid-19 pandemic, life expectancy had been steadily increasing across Europe in recent decades. This was due to a variety of factors, including reductions in childhood mortality, rising living standards, advances in medicine, and improvements in healthcare delivery [1].
However, this demographic shift towards longevity, coupled with lifestyle (e.g., work stress, poor diets, etc.) and environmental (e.g., pollution) stressors during adulthood have also led to a higher incidence of chronic conditions.
The pandemic has highlighted the chinks in the armor of European health systems. Acute care provision in several regions were pushed to brink of collapse. Furthermore, the strain on hospitals also had an impact on almost all other sectors of the medical field. Because of this, the European Union (EU) is not only working towards building the resilience of Member States’ health systems, but it is also continuing its work to strengthen health care delivery across the board, including supporting patients managing co-occurring chronic conditions.
While the latter has been ongoing for some time now, the stay-at-home mandates to curb infection rates underscored the need to accelerate the adoption of assistive technologies. Increasing investment in such technologies was originally motivated by rising healthcare costs and supported by research indicating that assistive technologies can help older patients gain more autonomy and live longer at home in a safe manner. However, over the course of 2020, it became clear that telemedicine and other digital health solutions were also important to protect elderly populations and people suffering from co-morbidities.
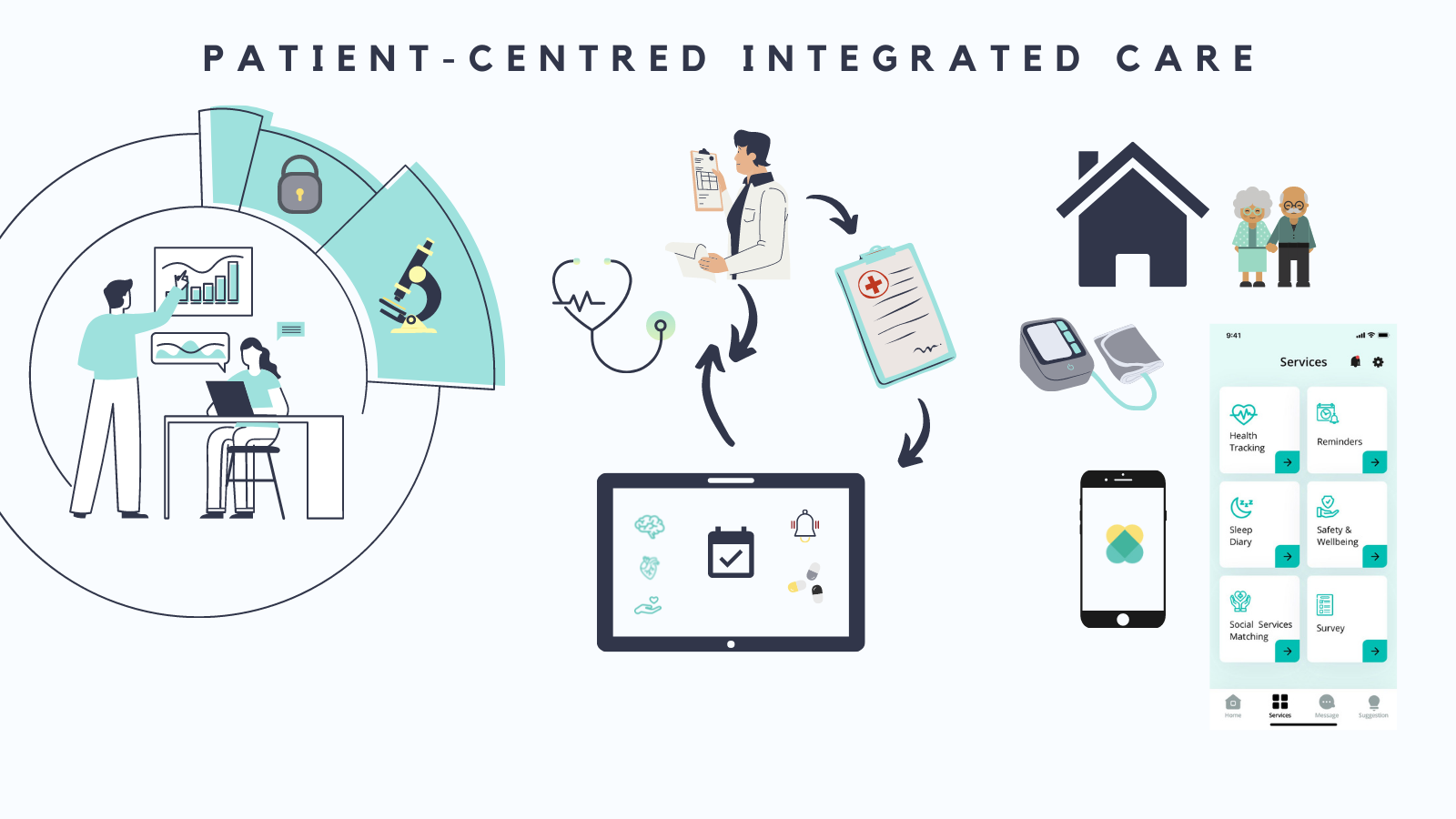
Today it is clear that integrated care supported by digital technologies is one way forward, but one with important caveats: it must be patient-centered, delivered in the framework of strong data protection and ethical safeguards, and it should complement interpersonal connections, not replace them.
Policy initiatives at the EU level
Over the years, the EU has created a comprehensive policy framework to improve the integration of health care delivery. The approach is multidisciplinary in order to cover the complexity of integrating care. It includes promoting medical and public health research, creating legal and ethical frameworks to protect sensitive information, strengthening Europe’s digital infrastructure, streamlining communication along patients’ care paths, and ensuring that the needs and requirements of patients are at the centre of it all.
The structure of and the work programme within Horizon 2020, and its successor, Horizon Europe, demonstrate the emphasis that has been placed on health in the EU. Assistive technologies and eHealth solutions in general are among the myriad of approaches Horizon 2020 and Horizon Europe help develop. For example, in the most recent work programme published in 2021, funding has been earmarked for research related to the ways in which we can use artificial intelligence to predict the risk of chronic conditions and track their progression. In addition, there are a whole range of calls to develop tools, technologies, and digital solutions that support patients managing non-communicable diseases, among other conditions [2].
Such research funds fit into the broader public health strategy led by the EU Directorate General dedicated to Health (DG SANTE). Its strategy for the first half of this decade highlights the important role eHealth can play across Europe. From reducing costs to helping catch triggers – which often occur outside clinical settings – that can lead to serious complications, the deployment of quality eHealth systems holds great promise.
It is important to note that the development of eHealth is occurring within a robust legal and ethical framework that includes the General Data Protection Regulation (commonly referred to as the GDPR), and new measures will be introduced to ensure that citizens across Europe have control over their personal data, including medical records [3].
Assistive Technologies are part of this integrated care ecosystem, but they are not silver bullets, and they cannot and must not be implemented in isolation. Rather, they should enable quality time for interpersonal relations.
REFERENCES
[1] Eurostat https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Mortality_and_life_expectancy_statistics
[3] See https://ec.europa.eu/info/system/files/sante_sp_2020_2024_en.pdf; more information on the foreseen creation of the ‘European Health Data Space’, p. 31.







